 Dental implantsDental implant surgery is a procedure that replaces tooth roots with metal, screwlike posts and replaces damaged or missing teeth with artificial teeth that look and function much like real ones. Dental implant surgery can offer a welcome alternative to dentures or bridgework that doesn’t fit well and can offer an option when a lack of natural teeth roots doesn’t allow building denture or bridgework tooth replacements.How dental implant surgery is performed depends on the type of implant and the condition of your jawbone. Dental implant surgery may involve several procedures. The major benefit of implants is solid support for your new teeth — a process that requires the bone to heal tightly around the implant. Because this bone healing requires time, the process can take many months.Conventional: A conventional implant is usually known as a ‘two pieces’ implant which consists of the root component and the tooth component in separate bits. Conventional implants come in a range of sizes to suit patients and can choose the most suitable implant based on the client’s needs and preferencesImmediate: Immediate implant placement means implantation at the same time instantly after extraction into the extraction socket. With this procedure, there is a reduction in the number of surgeries and shorten total treatment time.Missing tooth/ teeth replacement: An implant is a great way to replace a missing tooth. This solution feels and acts the most like a natural tooth when chewing, brushing or smiling. The implant replaces the actual root of the missing tooth and heals in the bone for several months.Mini dental implants: Mini-implants are a smaller version of regular implants. Typically, to be considered a candidate for regular dental implants, you must first have sufficient bone mass in your jaw. However, tooth loss causes bone loss, turning the situation into a vicious cycle. Mini implants help you to avoid the need for a bone graft, which requires several months on its own (up to a year) of healing.All on six /all on eight: All-on-6 implants an extra 2 implants to make the anchorage for the dental bridges to be tighter and more solid. Meanwhile, all-on-8 dental implants offer probably the maximum number of implants needed for restructuring your mouth and filling in all the missing teethSinus lift and bone graft: Sinus lift is a kind of bone graft procedure. It is performed when there is extreme bone loss on the patient’s maxilla (the part where the premolar and molar teeth are) or a pneumatized maxillary sinus (enlargement of maxillary sinus). This may require a bone graft as the sinuses are right above the upper teeth.Implant supported over dentures: An implant-supported denture is an oral appliance that replaces several teeth at once. It’s similar to a traditional denture. But instead of resting on top of your gums, an implant-supported denture attaches directly to your jawbone using dental implants. Dental implants are a popular and effective solution for replacing missing teeth. They are artificial tooth roots made of biocompatible materials, such as titanium or titanium alloys, that are surgically inserted into the jawbone to provide a stable foundation for prosthetic teeth.The dental implant procedure typically involves several steps:
Dental implantsDental implant surgery is a procedure that replaces tooth roots with metal, screwlike posts and replaces damaged or missing teeth with artificial teeth that look and function much like real ones. Dental implant surgery can offer a welcome alternative to dentures or bridgework that doesn’t fit well and can offer an option when a lack of natural teeth roots doesn’t allow building denture or bridgework tooth replacements.How dental implant surgery is performed depends on the type of implant and the condition of your jawbone. Dental implant surgery may involve several procedures. The major benefit of implants is solid support for your new teeth — a process that requires the bone to heal tightly around the implant. Because this bone healing requires time, the process can take many months.Conventional: A conventional implant is usually known as a ‘two pieces’ implant which consists of the root component and the tooth component in separate bits. Conventional implants come in a range of sizes to suit patients and can choose the most suitable implant based on the client’s needs and preferencesImmediate: Immediate implant placement means implantation at the same time instantly after extraction into the extraction socket. With this procedure, there is a reduction in the number of surgeries and shorten total treatment time.Missing tooth/ teeth replacement: An implant is a great way to replace a missing tooth. This solution feels and acts the most like a natural tooth when chewing, brushing or smiling. The implant replaces the actual root of the missing tooth and heals in the bone for several months.Mini dental implants: Mini-implants are a smaller version of regular implants. Typically, to be considered a candidate for regular dental implants, you must first have sufficient bone mass in your jaw. However, tooth loss causes bone loss, turning the situation into a vicious cycle. Mini implants help you to avoid the need for a bone graft, which requires several months on its own (up to a year) of healing.All on six /all on eight: All-on-6 implants an extra 2 implants to make the anchorage for the dental bridges to be tighter and more solid. Meanwhile, all-on-8 dental implants offer probably the maximum number of implants needed for restructuring your mouth and filling in all the missing teethSinus lift and bone graft: Sinus lift is a kind of bone graft procedure. It is performed when there is extreme bone loss on the patient’s maxilla (the part where the premolar and molar teeth are) or a pneumatized maxillary sinus (enlargement of maxillary sinus). This may require a bone graft as the sinuses are right above the upper teeth.Implant supported over dentures: An implant-supported denture is an oral appliance that replaces several teeth at once. It’s similar to a traditional denture. But instead of resting on top of your gums, an implant-supported denture attaches directly to your jawbone using dental implants. Dental implants are a popular and effective solution for replacing missing teeth. They are artificial tooth roots made of biocompatible materials, such as titanium or titanium alloys, that are surgically inserted into the jawbone to provide a stable foundation for prosthetic teeth.The dental implant procedure typically involves several steps:- Initial consultation: The first step is to visit a dentist or oral surgeon for a thorough examination and consultation. The dentist will evaluate your oral health, take x-rays, and determine if you are a suitable candidate for dental implants.
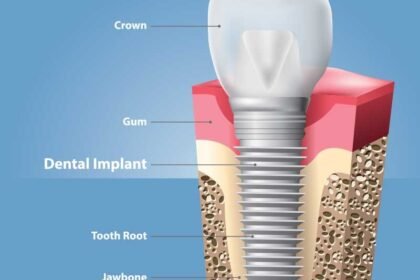
- Implant placement: During the surgery, the dental implant is placed into the jawbone beneath the gum line. Over time, the implant will fuse with the bone in a process called osseointegration, which provides stability and support for the replacement tooth.
- Healing period: After the implant placement, a healing period of several months is usually required to allow the implant to integrate properly with the jawbone. During this time, the patient may be given a temporary dental crown or bridge to maintain aesthetics and function.
- Abutment placement: Once the implant has integrated with the jawbone, a small connector called an abutment is attached to the implant. The abutment serves as the foundation for the replacement tooth.
- Restoration: Finally, a custom-made dental crown, bridge, or denture is attached to the abutment, completing the dental implant restoration. The new tooth is designed to match the surrounding natural teeth, providing a natural and aesthetically pleasing appearance.
- Endosteal implants: Endosteal implants are the most common type of dental implants. They are placed directly into the jawbone through a surgical procedure. These implants are typically in the form of screws, cylinders, or plates. After osseointegration, a dental crown is attached to the abutment, which connects to the implant, providing a natural-looking and functional tooth replacement.
- Subperiosteal implants: Subperiosteal implants are an alternative to endosteal implants and are used when there is insufficient jawbone to support traditional implants. Instead of being placed within the jawbone, subperiosteal implants are positioned under the gum tissue, but above the jawbone. They are custom-made to fit the individual’s bone contours and are secured on top of the jawbone. A metal frame protrudes through the gum, and the replacement tooth is attached to this frame.
- All-on-4/all-on-6 implants: These are a type of full-arch dental implant restoration. The “all-on-4” or “all-on-6” refers to the number of implants used to support a full set of upper or lower teeth. With this approach, a fixed denture or bridge is attached to the implants, providing a stable and permanent solution for individuals who have lost most or all of their teeth.
- Zygomatic implants: Zygomatic implants are used when there is severe bone loss in the upper jaw, and traditional implants cannot be placed. Instead of the jawbone, these implants are anchored into the cheekbone (zygomatic bone) to support dental restorations like bridges or dentures.
- Mini dental implants (mdi): Mini dental implants are smaller in diameter than traditional implants and are used in cases where there is limited bone width or to stabilize dentures. Due to their smaller size, they require less invasive surgery and may be a suitable option for some patients.
- Immediate loading/teeth-in-a-day implants: With this technique, the implant is placed and a temporary dental crown or bridge is immediately attached on the same day. This allows patients to leave the dental office with functional teeth while waiting for the final restoration to be placed after osseointegration is complete.
- Improved appearance: Dental implants look and feel like natural teeth, providing a seamless and natural smile. They are designed to match the color, shape, and size of your existing teeth, enhancing your overall facial aesthetics.
- Enhanced oral function: Dental implants function just like natural teeth, allowing you to eat, chew, and speak with confidence. Unlike removable dentures, implants are stable and don’t slip or move while eating or speaking.
- Long-term durability: With proper care and maintenance, dental implants have the potential to last for many years or even a lifetime. They are made of biocompatible materials like titanium, which integrates well with the jawbone, providing a strong and stable foundation for the replacement tooth.
- Bone preservation: When you lose a tooth, the jawbone in that area can start to deteriorate due to lack of stimulation. Dental implants mimic the function of natural tooth roots, stimulating the jawbone and helping to preserve its volume and density.
- Improved comfort: Dental implants become a part of your mouth, eliminating the discomfort often associated with removable dentures. They don’t put pressure on the gums or cause irritation.
- Better speech: Missing teeth can lead to speech difficulties. Dental implants restore your ability to speak clearly and confidently.
- Convenience: Unlike removable dentures, dental implants are fixed in place, so you don’t need to remove them for cleaning or worry about adhesives. You can brush and floss them just like your natural teeth.
- Adjacent tooth preservation: Dental bridges, another tooth replacement option, require the support of adjacent teeth. With dental implants, neighboring teeth are not altered or compromised, preserving their natural structure.
- High success rate: Dental implants have a high success rate when placed by a skilled dentist or oral surgeon and maintained with good oral hygiene practices.
- Psychological benefits: Dental implants can significantly improve a person’s self-confidence and self-esteem by restoring their smile and ability to eat and speak without embarrassment.